The healthcare industry is constantly evolving and advancing, and with these changes come new and more complex nursing roles. Advanced nursing roles require highly skilled and educated nurses to fill these positions. Advanced nursing roles not only require advanced knowledge and expertise but also the ability to work effectively with other healthcare professionals in an interprofessional practice. This article will explore the essentials of advanced nursing roles and interprofessional practice, discussing the importance of these roles and the skills needed to excel in them.
Advanced Nursing Roles:
Advanced nursing roles refer to a group of highly specialized positions within the nursing profession that require advanced knowledge and education. These roles can be broken down into three main categories: clinical nurse specialists (CNS), nurse practitioners (NP), and nurse anesthetists (NA). Each of these roles requires different levels of education and certification.
Clinical Nurse Specialist:
A clinical nurse specialist is an advanced practice nurse who specializes in a particular patient population or area of care, such as pediatrics, oncology, or critical care. Clinical nurse specialists work closely with other healthcare professionals to provide high-quality patient care, and they also play a vital role in the development and implementation of evidence-based nursing practices.
To become a clinical nurse specialist, one must have a master’s or doctoral degree in nursing, as well as certification in a particular specialty. Clinical nurse specialists are also required to have a valid nursing license and have completed a certain number of clinical hours in their area of specialty.
Nurse Practitioner:
A nurse practitioner is an advanced practice nurse who provides primary and specialty care to patients. Nurse practitioners can diagnose and treat illnesses, order and interpret diagnostic tests, and prescribe medications. They work closely with other healthcare professionals to provide comprehensive care to their patients.
To become a nurse practitioner, one must have a master’s or doctoral degree in nursing, as well as certification in a particular specialty. Nurse practitioners are also required to have a valid nursing license and have completed a certain number of clinical hours in their area of specialty.
Nurse Anesthetist:
A nurse anesthetist is an advanced practice nurse who provides anesthesia to patients undergoing surgical procedures. Nurse anesthetists work closely with anesthesiologists, surgeons, and other healthcare professionals to ensure that patients are safe and comfortable during surgery.
To become a nurse anesthetist, one must have a master’s degree in nursing and certification as a certified registered nurse anesthetist (CRNA). Nurse anesthetists are also required to have a valid nursing license and have completed a certain number of clinical hours in their area of specialty.
Interprofessional Practice:
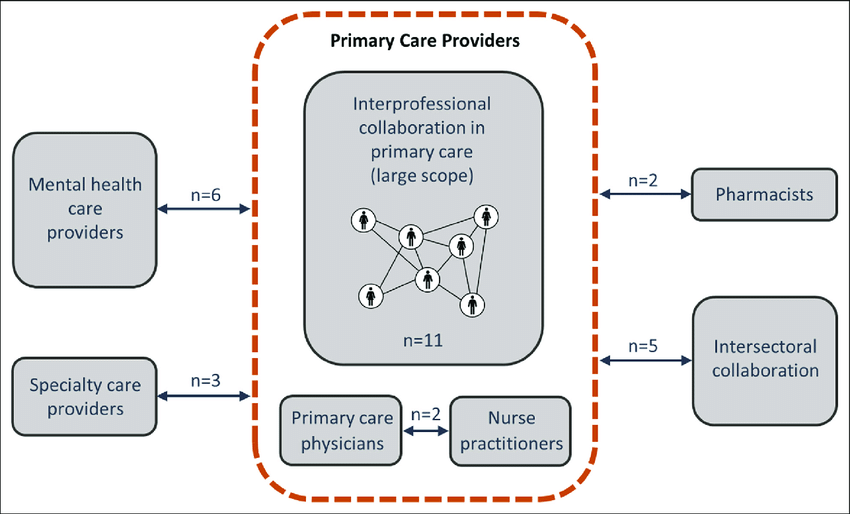
Interprofessional practice refers to the collaboration and teamwork between healthcare professionals from different disciplines to provide comprehensive and effective patient care. Interprofessional practice is essential in healthcare today because it allows for the best possible outcomes for patients.
The following are the essentials of interprofessional practice:
Interprofessional practice is a collaborative approach to healthcare in which professionals from different disciplines work together to provide patient-centered care. The following are the essentials of interprofessional practice:
- Communication: Effective communication is essential for interprofessional collaboration. It involves exchanging information, listening actively, and sharing knowledge and expertise with colleagues from different disciplines.
- Teamwork: Interprofessional teams work together to achieve common goals. They collaborate, cooperate, and respect each other’s roles and contributions.
- Roles and responsibilities: Each team member has a unique role and set of responsibilities that contribute to the overall care of the patient. Clear understanding and communication of these roles is critical for effective teamwork.
- Interprofessional education: Healthcare professionals should receive interprofessional education to learn about the roles and responsibilities of other disciplines, and to foster respect and understanding among team members.
- Patient-centered care: Interprofessional practice emphasizes the importance of patient-centered care, which involves involving patients and their families in the decision-making process and tailoring care to meet individual needs.
- Ethical and legal considerations: Interprofessional practice requires adherence to ethical and legal standards, including confidentiality, informed consent, and respect for patient autonomy.
- Continuous quality improvement: Interprofessional teams must continuously monitor and improve the quality of care provided to patients. This involves regular evaluation of outcomes, feedback, and communication among team members.
Overall, interprofessional practice is a collaborative approach that emphasizes teamwork, effective communication, and patient-centered care to provide high-quality healthcare to patients.
Find online help in writing essays, research papers, term papers, reports, movie reviews, annotated bibliographies, speeches/presentations, projects, presentations, dissertation services, theses, research proposals, essay editing, proofreading, Book reviews, article reviews, formatting, personal statements, admission essays, scholarship essays, application papers, among others.

 WRITE MY ESSAY NOW!
WRITE MY ESSAY NOW!